Hospital de campaña, Wuhan (China)
It is fitting to use the name of the nurse Isabel Zendal, a key figure in the extraordinary expedition that took the smallpox vaccine to the confines of the Spanish Empire early in the 19th century, for the Community of Madrid’s new hospital for epidemic diseases. The tribute is parallel to the one that NHS England paid last April, when the centers set up for coronavirus patients were named in honor of the country’s most famous nurse and author of Notes on Hospitals, Florence Nightingale.
But the new Isabel Zendal Hospital, like almost all projects, decrees, and operations born out of the pandemic of 2020, has become an object of controversy. Controversies in the year of Covid-19 rarely generate true debate. They instead are presented as dilemmas, subject to praise or condemnation. The new facility follows this tendency fostered by media, networks, and parties or the so-called political class. And, as in similar cases, opinions on the matter in dispute will be extracted from a range of professionals – physicians, economists, architects –who, chances are, were neither informed about the project, let alone consulted, so their arguments in favor of or against it are not really solicited to generate truly useful deliberations.
We ought to consider a matter that stands out over the dark void which the unsustainable structure of expenses incurred by the health system is. Isabel Zendal is not simply one more hospital, not just another hospital of the system. It is not even a hospital, at least not in the sense we know, but an emergency center, or a huge ICU with lots of beds, and as such, it has more in common with a refugee camp or the Kalighat Home for the Dying in Kolkata than with our public hospitals where people are confined or our health system’s specialist centers. It does not have their programs, their complex treatments, or their objectives. For its purpose is not to cure citizens afflicted with the strange mutant virus – something no one knows how to do, so no one for the time being can achieve – but to isolate them, and in so doing, save the system from paralysis. To preserve the system’s hospitals, the major hospitals of scientific medicine that have had to abandon the populace for months, that have postponed surgeries, that already have more than enough on their hands battling their own insurmountable bacteria. Obviously the mission of Isabel Zendal Hospital is to save the lives that depend on being treated in Madrid’s hospitals, so it is wrong to think it an alternative to reinforce human resources or technicians in the latter, themselves paralyzed by a virus they cannot combat but just deal with as best they can.
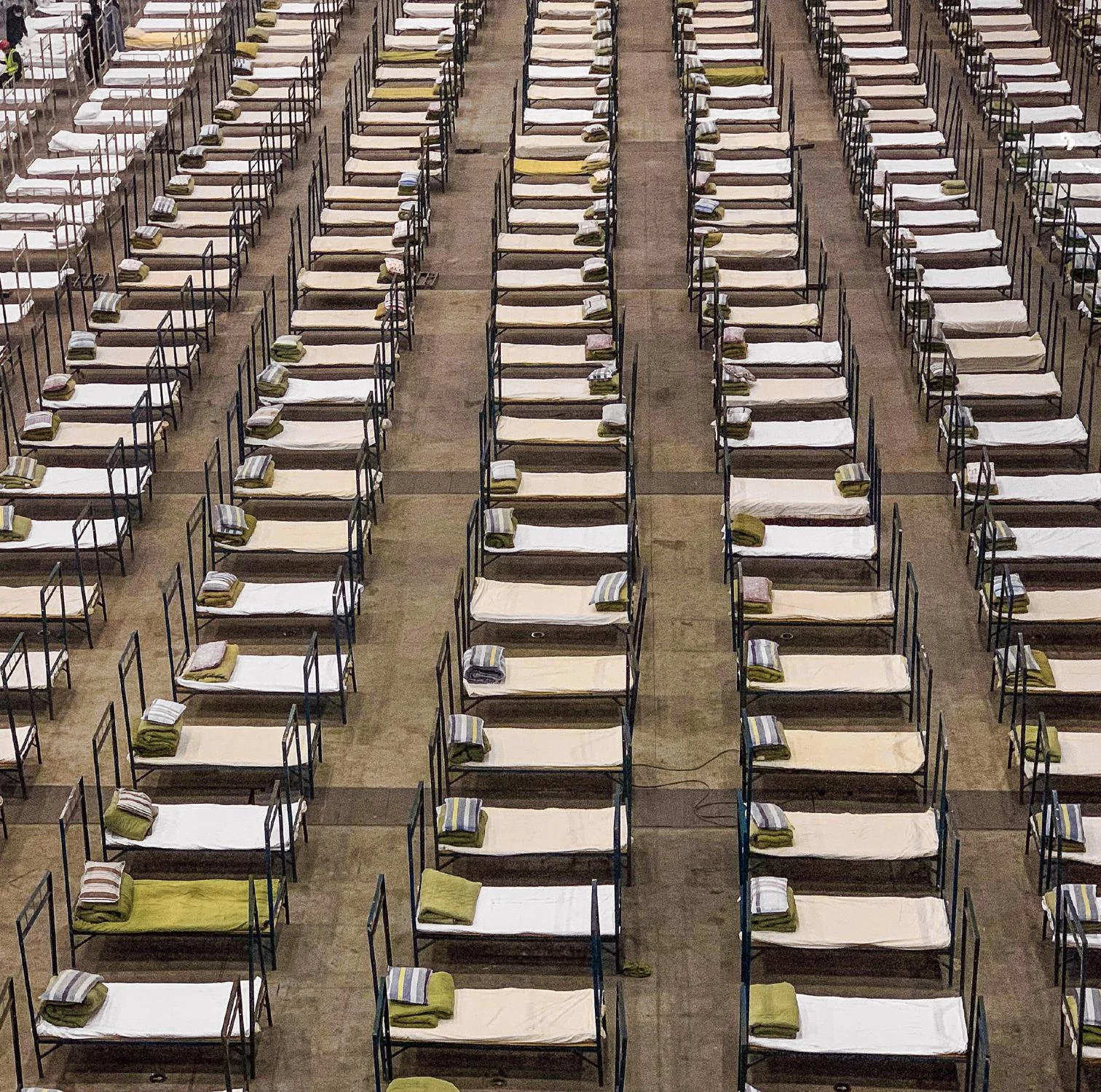
The explosion of the virus in Wuhan showed us early on that the pandemic would require improvising huge volumes and areas to accommodate hundreds of beds, similar to the ones set up in the wake of natural catastrophes like floods and earthquakes. The construction in record time of a giant modular and medicalized container right where the virus originated, a much publicized fact, seemed to point to a single possible solution: enormous emergency facilities minimally provided with diagnostic equipment and treatment material, quite like a 1950s first-aid station. But that precedent was not well received amongst us. Suddenly, and against all odds, it meant returning to the hospital of infectious diseases of yore, to that place invented in the Early Middle Ages to fight successive and recurring plagues imported from the East. That building where Italian republics confined the ill to keep them away from the city, the same institution for the infected that was a fixture outside all European capitals until the advent of antibiotics.
From the 1980s onward, the hospital became more and more a center for medical procedures and consultations and less and less a place for confinement, moving toward the ideal of the bedless hospital. And now, when it makes no sense to measure the capacity of the sanitary system by number of beds, as in 1950, what we need is a building for thousands of beds and very limited, specific treatments. The distressing problem for the health authorities is that we are once again faced with a medieval plague, and are at a loss to beat it. And they deem inevitable a medieval solution, an isolated hospital for the infected. Alas, the plague is back and is here to stay, and we must accept this if we want to prevent, from now on, what any other Wuhan could easily put in circulation. And so it was that by repurposing halls of IFEMA, Madrid’s trade fair premises, a field hospital was set up to take in infected people. It was like the English solution in the Nightingale hospitals, also with beds numbering between 500 and 5,000. Neither the Madrid nor the Wuhan field hospital drew media attention to its basic architecture; in both cases, journalists were focused on sanitary and political aspects. Any instance of quick construction through emergency methods can be of some technical interest, but is not that newsworthy.
The foreseen second wave of the coronavirus, by now a usual visitor, laid bare the unpreparedness of our health system. In the chaos, the government of the region of Madrid has demonstrated an incapacity to even digest the challenge of a global future that mutant viruses pose, as this does not fit into any of its sanitary or philosophical presuppositions. It has hardly reacted other than to demand more funds from an administration which is ever reluctant and opaque in matters having to do with hospital expenditure. Isabel Zendal is an improvised response that endeavors to accept the aforementioned Wuhan way, and tries to pursue the positive experience of IFEMA, barring the inconveniences presented by an extemporaneous installation in a trade fair complex. Remember that for a hospital of the system, the cost of construction is close to that of a year of being operational. The project almost literally reflects the solution adopted in the two repurposed IFEMA pavilions, dividing about a thousand beds into three groups. While the functional program has been redacted by the IFEMA team itself, it is a direct application of the precedent, even in the organization of the space, from the huge hall to the plain container, with little elaboration.
The project was divided into three parts, each urgently carried out by a firm with its own experience and degree of antiquity in designing hospitals for the health system. The actual hospital, executed in three confinement blocks or modules, was assigned to Chile15 (Alberto Jorge). A pavilion for administrative services and a general storage for medical material were commissioned to Aidhos (Alfonso Casares and Reinaldo Ruiz Yébenes) and Árgola (Luis González Sterling), respectively, and each part or module of the building was to be allocated to a contractor. The suitability of the architectural project is of course arguable, and we will have to dole out pass and fail marks on the chosen model among those who laid down the program and the team that interpreted it and its precedents, because public architecture must give the best service possible. There will always be the alibi of improvisation, of rush jobs, and of the opacity of administrations when hospitals are concerned, but this is something that architects of hospitals are accustomed to, so should be able to deal with. It is alright to wonder if the triple container of the IFEMA kind – a huge space with beds arranged in rows, as in a field hospital, supposedly for short to medium confinements – is the best model for tending to the sick and for the wellbeing of patients and medical staff alike. But there are other issues at stake.
The Isabel Zendal debate would be useful if it included discussion on how to equip an epidemic hospital and its staff for both discontinuous and permanent operations, and on its role in both competing and collaborating with the pair formed by confinement hospitals and primary health centers, a marriage resulting from current healthcare laws. Because it does not seek to be a confinement hospital in the usual sense, nor a reserve or long-confinement hospital, but a temporary place for victims of an epidemic that cannot be treated as a regular hospitalization case, it has to probe for a provisional function and a commensurate level of maintenance. But the very hospital-health center partnership remains inefficiently organized in its functions, connections, powers, and budgets within the sanitary system, which is proving increasingly unsustainable. So the debate has a confusing backdrop.
Justo Isasi has written La arquitectura de la ciencia médica. The Architecture of Medical Knowledge (CEU, 2013).

Chile15 Arquitectos, Hospital Enfermera Isabel Zendal, Madrid





